Provide rapid, person-centered intake and a complete care plan within 72 hours of the date of request. This thing works to help veterans engage early, set expectations, and accelerate access across primary care, mental health, and social supports. The process is designed to be transparent, with a dedicated case manager who tracks milestones and follows up promptly.
Our programs span medical, mental health, and social services, and they address the needs of families as well as individuals. For veterans with adolescent dependents, we offer family-focused counseling and school-linked supports to reduce secondary stress. Our experienced team, and therefore a collaborative approach, tailors services to each person, not to generic templates.
Following intake, conduct a complete, multidisciplinary assessment to identify strengths, risks, and preferences. We combine medical screenings, mental health evaluations, and psychosocial planning. The team ensures cases are handled by a multidisciplinary group using evidence-informed, nonrandomized approaches that emphasize patient safety and autonomy. We document a complete plan with clear dates for review and adjustment.
Evidence from johns programs shows that integrated, veteran-centered care reduces hospitalizations and improves completion of services. In nonrandomized, real-world studies, a coordinated approach across primary care, behavioral health, and social supports achieved a 20–30% reduction in emergency department visits within 6 months and a 15–25% increase in program completion among veterans with co-occurring conditions. Findings reflect experience from diverse clinics and are tracked with regular updates on the date of review to guide adjustments.
To implement this model, clinics standardize intake within 72 hours, maintain trauma-informed and nonviolent care, and integrate toxicity screening. A dedicated care team handles each case, including peer mentors, and records progress in a shared plan. Schedule check-ins every two weeks for the first two months and monthly thereafter, ensuring following steps are documented and followed. Partnerships with johns programs and community providers help sustain access to treatment, including medication-assisted therapies when appropriate.
How to enroll in VA health care and book your first appointment
Apply online at va.gov to enroll in VA health care today. Create your account, enter your service details and contact information, and submit the enrollment form (10-10EZ) or an equivalent request. Have your proof of service (DD-214), a government ID, and your current address ready; you can upload these documents or mail them if needed. The portal provides a definition of eligibility and a timeline for processing. Across america, united states veterans use this route to access care, including those in pittsburgh who want to connect with the VA Pittsburgh Healthcare System. If you were transferred from another facility, mention the transfer so your records can be linked.
Enrollment: how to begin
Choose your path: online at va.gov, by phone, or in person at a VA facility. Gather specified documents: DD-214, photo ID, proof of address, and any records from civilian providers. Complete and submit the enrollment form; ensure the information is entered accurately. If you were transferred, provide transfer details to link records. List chronic conditions such as hepatopathy so the care team can plan appropriately. If you have medication lists, include topotecanmgm to help reviewers assess drug interactions. You may need to order records from civilian providers to speed review. If you have a misdemeanor on file or court records, discuss with a VA benefits counselor to understand implications. After submission, monitor the status in the portal or through the enrollment line.
Booking your first appointment
After you’re enrolled, book your first appointment through the My VA Health portal or by calling your local VA scheduling desk. The online system supports an e-commerce style flow to choose primary care or specialty services and pull in preferred times. In pittsburgh, the VA Pittsburgh Healthcare System scheduling team, including Turner staff, can assist with access and transfers. If you need family care or childrens services, request the appropriate clinic and note any chronic conditions to tailor your plan. Bring your photo ID and enrollment confirmation to the visit; if you have alcohol use concerns, you can discuss treatment options during scheduling so they are considered in your plan. If your move requires record transfer, request that records be entered into the new facility’s system. You can cancel or reschedule via the portal or the scheduling desk if your plans shift. Your first appointment lays the groundwork for a stronger, coordinated care experience across the united health network.
What to know about crisis, PTSD, and trauma care: immediate steps to get help
Call your local crisis line immediately if you or someone you know is in danger. In your country, dial the local emergency number or 988 in the United States; text or chat options are often available 24/7. This is the completed first step toward safety.
Stay with the person, remove hazards, and keep conversations calm. If possible, connect them with a trusted contact and ask that person to come to the scene. Early action reduces escalation and helps you count on a clear plan rather than acting alone.
Seek a crisis evaluation as soon as possible. If urgent, go to the nearest ER or VA facility for stabilization. Some clinics use an irs-iii intake guide to gauge urgency and plan next steps. If you prefer therapy or other approaches, request options that fit your needs; care can proceed with or without therapy depending on the setting.
Note possible medication histories, such as dactinomycin, and discuss with the clinician if relevant to safety or symptoms. These details help the team tailor your plan.
In a courtroom context, a defendant who served in the military can still access crisis support. Guidance from a peer or clinician helps you craft a safety plan that you can follow back home.
For trauma care, begin with psychoeducation, grounding exercises, sleep hygiene, and gradual exposure when appropriate. Short, regular strategies–like a five-minute grounding routine–can reduce distress. A well-structured plan can reduce the risk of relapse and support ongoing care, with steady progress across the patient population.
Engage your support network: family, friends, or veteran peers. stephanie, who served four-year in the Air National Guard, shares how peer support and guidance from a trusted clinician helped her feel better and stay connected. Remember that violations of trust or trauma history can complicate a crisis; seek appropriate support and, if needed, legal guidance.
Be aware of tampas–barriers like stigma, transportation, and wait times–that slow access to care. Include a backup contact in your plan and a safe place to go if the primary option is unavailable. Start from the beginning of care and build a steady routine that you can maintain in daily life. In a four-year span of service, many veterans count on these steps to regain control and safety.
Keep notes on your progress: sleep patterns, days with functional ability, and flare-ups. This data helps clinicians tailor care for patients across different stratum of functioning and can inform a moving plan toward stability and wellness.
Care pathways and how to access help
| Zdroj | What it offers | How to reach | Najlepšie pre |
|---|---|---|---|
| Veterans Crisis Line (US) | 24/7 confidential crisis support for veterans and families | Call 988 and press 1; chat at veteranscrisisline.net | Immediate crisis support |
| VA Medical Centers / Vet Centers | In-person evaluation, stabilization, and ongoing PTSD care | Find a center via va.gov or call 1-800-827-1000 | Ongoing clinical care |
| Local emergency services | Immediate safety assessment and stabilization | Call your local emergency number; go to the nearest ER | Severe danger or self-harm risk |
| Peer-support programs | Early, non-clinical guidance from veterans peers | Contact local veterans organization or hospital social work | Navigation and social support |
Locating in-home and community-based rehabilitation services
Call your VA care coordinator to request a central directory of licensed in-home and community-based rehabilitation services within 25 miles and set up an initial evaluation within two weeks. This concrete step creates a baseline for comparing options and speeds up access to care.
Practical steps to identify suitable providers

- Ask for a four-provider shortlist that covers home-based primary care, in-home physical and occupational therapy, and speech-language pathology; confirm each option is licensed and accepts VA referrals.
- Review the subtype of services offered (physical therapy, cognitive rehab, skilled nursing support) and how often visits occur; verify whether tele-rehab is available if travel is limited.
- Check proximity and transportation plans; ensure the provider can visit the home and also support visits to central sites if needed, especially for complex cases.
- Review records and pre-visit data: medical history, surgical notes, intracranial events, creatinine results, current medications, and the latest care plan; if records were transferred, verify they arrived in full and are accessible.
- Coordinate transfer of records from previous providers; confirm data privacy, the necessary consent forms, and that records can be accessed quickly by the new team.
- Ask about start date estimates and what the initial assessments will cover; request a written plan with goals and a two-sided contact sheet for the veteran and caregiver, including the White River Junction area if applicable.
- Inquire about costs, insurance coverage, and VA program participation; request an estimated cost outline and a plan to address any gaps in funding.
- Clarify whether the team can order therapeutic devices or home modifications if needed to support independence, and who handles these orders on the central care team.
Checklist before enrollment
- Confirm licensing and any accreditation required by state or VA programs; verify the provider’s current status and staff credentials.
- Ensure the rehabilitation plan matches the veteran’s understanding of goals, including back-to-work or career objectives and personal independence milestones; does the plan address urgent needs and escalation procedures?
- Assess home safety and readiness: fall risk, lighting, stair access, grab bars, and any necessary equipment; document what can be funded or subsidized.
- Set a practical schedule: number and frequency of visits, two-sided consent forms, and backup options if transportation or caregiver availability changes.
- Confirm documentation: order of therapy sessions, progress notes, and how records are stored; ensure a central file is maintained and updated for all providers.
- Plan for coordination with other clinicians, including surgical or intracranial considerations; ensure the plan does not clash with existing medications or therapies and aligns with the veteran’s health record.
- Establish emergency protocols and primary contact information; create a back-up plan for weather or transportation disruptions and ensure the veteran’s records can be transferred quickly if needed.
- Ask about long-term options that support a gradual return to daily activities or a new, suitable career path; confirm the estimated year when stepping down or transitioning to less intensive services is discussed.
Practical guide to housing support and benefits for veterans

Take action now: submit your failure-free housing benefits claim to the national veterans program within 30 days of discharge. Gather DD214, proof of income, recent utility bills, and a doctor’s note if you have a health condition such as rhabdomyosarcoma; including a clear statement of needs strengthens the case and speeds processing, andor additional supports may be requested.
As the author, I offer advice on steps that reduce delays: check eligibility for a housing allowance, a grant for home modifications, and rental subsidies; you can apply through the national portal or at a local service center, and always keep copies of every submission.
Pre casey, a veteran with a služba history and a condition requiring modifications, start with a service verification letter and a medical plan showing the need for adaptations. Submit these with the housing form to unlock secondary benefits like grants and subsidies throughout the home retrofit.
Ak ste retired from active service, indicate pension, disability, and any federal benefits to establish income limits and rent consideration. The effect on your housing cost guides the order of subsidies and the plan you pursue; this helps prevent miscalculations and delays.
Expect cycles of review: after initial approval, annual updates may be required; some programs use a 5-year cycle to recheck eligibility, with national policy updates that may affect what you qualify for during induction of new guidelines.
Beyond rent support, explore opportunities such as energy-efficiency upgrades and accessible alterations funded by grants. In practice, porovnať options and note how compared programs differ in eligibility and timelines. Compared to private housing, these options provide stability; use a simple order of needs checklist to decide what to pursue first, then align with your local timelines and budget.
Throughout the process, keep a secure file, note deadlines, and seek support from a trusted advisor who can provide quick feedback and help you avoid common errors.
Finding peer support networks and veteran-friendly clinics in your area
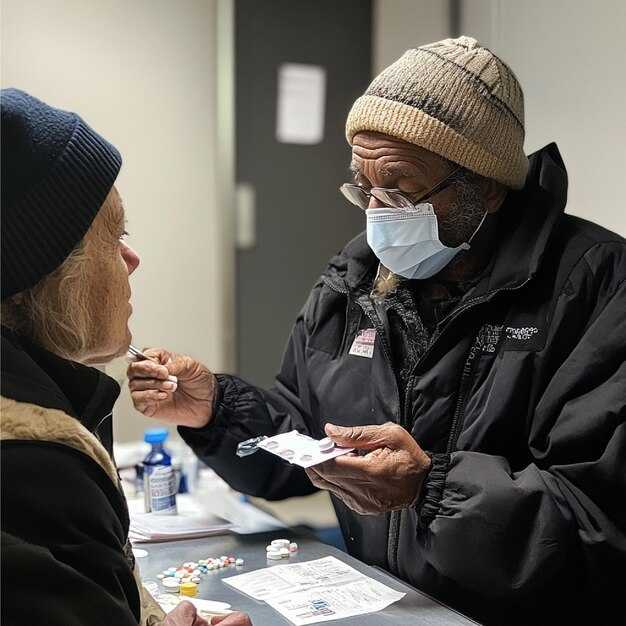
Take the first step by contacting your local VA medical center or Vet Center to obtain a personalized list of peer support networks and veteran-friendly clinics in your area, and ask for referrals to patient-centered programs that focus on processing trauma and life after service.
Map out options by calling official directories and speaking with coordinators; in most regions there are at least 4–6 peer groups with weekly talk sessions, and over 60 percent of participants report feeling less isolated after three months.
Look for veteran-friendly clinics that have a dedicated care team, flexible appointment times, and telehealth options; this service mindset reduces no-show rates and improves continuity of care, especially for patients with mobility or transportation challenges.
Family support matters: pediatric social workers can coordinate with veteran mental health care to support dependents, creating a family-centered approach that extends well beyond the patient.
james, a participant, describes how weekly talk circles hosted by the rodeberg group gave him a safe space to discuss abuse experiences and to practice processing; like many participants, he found that speaking with peers who understand service life keeps him connected and moving forward.
Despite common barriers such as transportation or work schedules, veteran-friendly clinics that coordinate with oncology, primary care, and social work teams can support patients receiving treatments like cyclophosphamide, ensuring psychosocial care accompanies medical care.
In analysis of regional data, providing structured peer support alongside formal therapy correlates with higher retention in care and lower crisis calls; in cases with elevated risk factors, peer networks can reduce the risk of death by suicide; this holds for PTSD, extremity injuries, and chronic pain cases.
Justice services and benefits navigation support reduce barriers to care; ask clinics about on-site justice resources who can help with claims processing and appeals, increasing chances of successful outcomes.
Processing trauma takes time, but you are not alone; taking this step is giving you options to support processing and life rebuilding, therefore you can regain momentum and purpose.
Featured stories: real veterans sharing paths to care and recovery
Connect now by contacting your regional veterans affairs office to be assigned a certified care team that follows national guidelines; this action provides a right starting point during the first 30 days of care.
casey, a veteran from nebraska, faced a cancer diagnosis and toxicity from treatment. A regional, multidisciplinary team assigned to him crafted an original care plan that included clinically guided radiotherapy, toxicity monitoring, and psychosocial support. Mentors supported the process, with approximately twelve weeks of treatment and follow-up visits to ensure the patient was back to daily activities.
Those with diverse backgrounds access care through a national framework that coordinates regional clinics with certified therapists; when veterans need help with PTSD, pain, or exposure-related effects, a coordinated plan reduces delays and improves adherence.
According to nebraska data, approximately 68% of patients receiving integrated medical and psychosocial care clinically show improved functioning within three months.
During the process, clinicians explain the erms and rights clearly, and the original consent documents are stored to support consistency when assigned clinicians rotate.
After radiotherapy and ongoing toxicity management, casey rejoined his career path with support from his regional team and a care plan that included regular follow-ups at clinics across nebraska.
Those seeking support can take concrete steps: contact regional offices, request a certified team, verify the assigned case manager, and schedule a clinically supervised assessment within two weeks when possible, ensuring a sustained action plan that respects need and rights.


Komentáre