
Implement a joint Pavlov Medical–University programme in warsaw as a three-year initiative that blends clinical training with translational research and patient-focused experience.
Establish a cross-institutional steering group led by yaremenko そして plouzhnikov, with ministry representation, to co-design curricula, assessment methods, and research blocks within the programme.
For the first cohort, recruit 60 students across three tracks: anesthesia, biomedical research, and education technology, and embed a lambing project in obstetrics to test field deployment and data collection.
Schedule a kickoff 訪問 にある。 15th day of the quarter to approve the collaboration and launch the first module, with milestones defined for teaching hours, clinical rotations, and initial publications.
Use an nprove metric to measure early outcomes, including hours of training completed, simulation scores, and number of co-authored papers, and share results with the ministry and affiliated hospitals to guide scaling.
Develop a sustainable promotional plan that highlights patient-centered training, offer internships for residents, and invites external experts to visit the warsaw sites, then surf between teaching labs and hospital wards to gather real-time feedback and improve the programme.
As a next step, invite warsaw partners to review progress after the first year and set a plan for expansion with more programme components and joint research topics, ensuring experience-based learning informs policy and curriculum at both institutions.
Transition Governance: Decision Rights, Steering Committee, and Timeline
Establish a formal Transition Governance framework with defined decision rights, an 18-month timeline, and an active Steering Committee. The model takes surgical training, cross-specialties collaboration, and research alignment and channels them into a cohesive program that benefits doctors and students more than before.
Decision rights specify who can approve curricular changes, budget allocations, risk policies, and patient-safety standards. The process uses a registration point to capture every approved modification, ensuring version control and accountability across programs. When clinicians come together, the work remains focused and auditable.
The Steering Committee should include member representatives from clinical specialties, a resident or fellow, a data liaison, and an external adviser. dear colleagues from administration and patient-facing services contribute, and contact details are published in the project hall to enable quick guidance and continuous feedback. The framework promotes organic collaboration across centers and ensures any profit from ancillary activities is reinvested into learning resources.
Engagement and transparency rely on community channels. A reddit thread and a forum invite input from doctors, patients, and regional partners in uzbekistan and zealands, with all-russian standards guiding every decision. A fisherman example from a coastal hub shows how outreach must adapt to field practice, while awarded funds support pilots and learning sessions. The aim is to gather learning beyond the class hall and convert it into structured action.
Tools and data flows include an e-diary that tracks learning milestones, vaccination status, and retaking opportunities for remediation. A contact point for stakeholders ensures rapid responses. Teams forage insights from real-world practice to inform next steps, while the hall becomes a shared space for governance work.
| Milestone | Timeline | Owner | Decision Rights | Output |
|---|---|---|---|---|
| Governance charter approved | Q1 | Steering Committee | Approve charter; register changes | Charter document |
| Curriculum modification proposal | Q2 | Academic Board | Approve modifications; register updates | Registered modules |
| Data framework for e-diary and vaccination | Q3 | IT & Learning Services | Approve data schema; privacy controls | Integrated data system |
| Pilot cross-specialties program | Q4 | Clinical Leads | Approve pilots; allocate funds | Pilot results |
| Regional partnership plan (uzbekistan, zealands, all-russian alignment) | Q5–Q6 | Partnership Office | Authorize collaboration; registration of partners | Partnerships list and milestones |
Curriculum Redesign: Core Clinical Skills by Year and Integrated Assessment
Recommendation: Build a four-year, competency-based curriculum with a clear skill ladder and an integrated assessment framework that binds early patient-facing work to ongoing feedback and explicit milestones. Allocate dedicated simulation hours, clerkship blocks, and interprofessional seminars to support confidence-building before real-world tasks.
- Year 1 – Foundations of clinical observation and communication
- Hours: 180 hours clinical contact; 40 hours simulation
- Core skills: history taking; focused physical examination; structured documentation; patient safety and infection control; professional etiquette; basic ethical reasoning
- Assessment: six OSCE stations; regular observed encounters with structured feedback; a starting reflective portfolio entry
- Year 2 – Expansion of examination and procedural skills
- Hours: 210 hours clinical rotation; 60 hours simulation
- Core skills: expanded system exams; venipuncture; wound assessment and aseptic technique; management planning; interprofessional communication
- Assessment: eight OSCE stations; Mini-CEX in ward settings; procedural checklists; portfolio entries with case analyses
- Year 3 – Integrated rotations and diagnostic reasoning
- Hours: 240 hours clinical time; 80 hours simulation
- Core skills: differential diagnosis; test selection and interpretation; imaging basics; telemedicine encounters; teamwork and ethics in management
- Assessment: twelve OSCE stations; WBAs for real cases; structured case write-ups; reflective entries
- Year 4 – Capstone, transition, and readiness for practice
- Hours: 240 hours clinical time; 100 hours simulation and project time
- Core skills: leadership in clinical teams; supervision of junior learners; evidence-informed management plans; crisis resource management; patient and family communication in complex scenarios
- Assessment: final OSCE with integrated scenarios; culmination portfolio review; oral viva on a capstone project; handover of a comprehensive patient case log
Integrated assessment architecture binds the four-year program with a multi-component framework. Components include:
- OSCE progressions: six, eight, twelve, and fourteen stations across Years 1–4
- WBAs: Mini-CEX and DOPS conducted during routine encounters
- Structured portfolios: reflective entries and case analyses across modules
- Knowledge checks: system-aligned quizzes and short-answer tasks
- Capstone project and oral viva: year-4 culmination
Research-Teaching Bridge: Structured Projects, Co-mentored Students, and Lab Rotations
Adopt a three-track Research-Teaching Bridge: structured projects with milestone-based reviews, paired co-mentors, and lab rotations. Define a term-by-term project slate with clear objectives, timelines, and a transparent evaluation rubric, and specify the order of steps from plan, through execution, to analysis. This design replaces ad hoc experiences with defined deliverables and explicit progress checkpoints that guide students from hypothesis to preliminary data, where mentors ensure alignment.
Each project takes a defined scope and uses waterproof briefs to standardize expectations. Pair an associate mentor from Pavlov Medical with a clinician from otorhinolaryngology-head to ensure clinical relevance and cross-disciplinary insight. Schedule quarterly visit days to mix bench and clinic exposure; these visits connect students with clinicians, data teams, and patient-facing researchers. Include molecular components when suitable, and added a ddshostakovich-inspired notebook for structured coding and data notes to support reproducibility.
Rotations deliver hands-on experience across three labs in four-week blocks, allowing students to surf through techniques, compare approaches, and identify mentors aligned with their interests. Track progress with a weekly update digest and a shared dashboard, reinforcing memory of methods and data workflows. Host an annual event, the 15th edition of a university internal symposium, where teams present posters and some projects are awarded micro-grants or travel support. Invite friends from related programs to broaden discussion, allocate times for feedback, and welcome a Luxembourgish exchange student into the cohort. Plan another iteration in the next term and apply this model to additional departments to scale impact around campus.
Clinical Training in a University Setting: Clerkships, Sim Labs, and Rural Rotations
Implement a centralized, competency-based curriculum that unites clerkships, sim labs, and rural rotations under a single governance framework. This approach pins every milestone to real-world outcomes in dentistry and medicine, ensuring your students meet primary care competencies while collaborating with colleagues across sectors. Start with a two-track ramp: urban clerkships for hands-on patient care, plus sim labs for procedural mastery; then integrate rural rotations to expose learners to distance challenges and population health needs. Publish a simple click-through guide that outlines sites, rotation lengths, and assessment criteria, and refresh it every september to reflect local capacity and new accreditation standards. Provide a quick click to the portal for the latest updates.
Clerkships deliver direct patient contact in urban city hospitals and community clinics. Design eight-to-twelve-week blocks, pairing each student with a primary mentor team to support becoming confident clinicians. Use rotation itineraries that balance dentistry procedures with general medicine encounters, ensuring clinical reasoning is tested through real cases. Maintain consistency by linking sites to the central information system, and include opportunities in vaskelovo and aran partnerships to broaden exposure to diverse patient populations, including international students. Ensure distance travel plans have defined accommodations and safety checks, so no learner is disadvantaged.
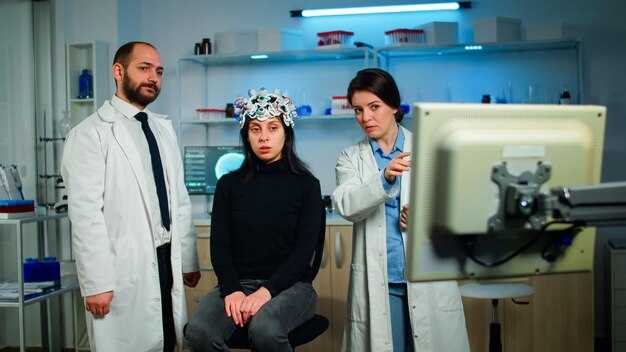
Sim labs stand as a powerful ツール for skill building. Use high-fidelity mannequins and virtual simulators to practice suturing, injections, radiography, and exam techniques before real patients enter the room. Create standard scenarios for dentistry and medicine, and collect immediate feedback through structured debriefs. This innovation pathway supports creating a shared mental model among students and colleagues, and laboratories can be awarded accreditation by the sector’s standards body when criteria are met. Include information about performance benchmarks in the student portal to guide your learning progress.
Rural rotations connect classroom skills to community health needs. They emphasize primary care, preventive services, and the social determinants of health in settings far from the city. They are four-week blocks at rural sites with well-defined supervision and remote support. This model is inspired by long-standing rural training traditions and respects 19th century roots of clinical training, adapting them for modern rural care. Use distance learning to maintain continuity with urban mentors, and organize monthly case conferences that include sheepmeat producers and local veterinarians for One Health collaborations. Plan for a september cycle and align with the academic calendar to maximize student engagement and inspiration.
Assessment and outcomes: gather data on procedures performed, complication rates, and patient satisfaction. This data clarifies the need of each learner and helps tailor coaching. Use a centralized dashboard to compare clerkship and rural rotation metrics across sites, including urban and rural, to identify gaps and opportunities for improvement. The leadership decided to award additional support to sites delivering high-quality, interdisciplinary care, reinforcing your central mission to place patients first. Include information about best practices in the portal so learners can plan their next steps, and ensure that the needs of participants are met, including provisions for those balancing distance travel and clinical duties. This is very important for equity and access. Share results with colleagues and students to drive continuous improvement, and ensure information is accessible and actionable for all involved.
Assessment Framework: Competency-Based Progression and Real-World Milestones
Adopt a competency-based progression that ties stage completion to observable clinical performances and patient outcomes. Use a central rubric that measures mastery across core domains–history taking, physical examination, procedural skills, medical decision making, and professional communication. Prioritize real-world milestones from diverse settings to reduce bias from single-site assessment, and implement structured evidence collection in outpatient clinics, wards, and telemedicine encounters. Where resources are limited, adjust milestones to practical tasks. Pair tests with a longitudinal portfolio and peer-review discussions. Include gynecology and womens health scenarios to reflect gender-specific care and align with 19th-century to modern teaching principles, showing how a wider spread of knowledge supports learners. Drawing on petrograd traditions informs our peer-review approach. Involve learners from the largest teaching hospitals to spread proven practices.
Design and governance
Establish central governance: a panel of colleagues from medical disciplines, including gynecology and womens health, to supervise progression, calibrate rubrics, and coordinate cooperation across sites. Run quarterly forums and an event-based review process to discuss difficult cases and ensure alignment with republican health policies. Use a plouzhnikov-inspired case bank to diversify scenarios, and reference petrograd-era teaching forums to design peer-feedback loops. Track data from the largest teaching hospitals to spread successful practices to smaller programs. Capture feedback via a simple form and let learners click to submit evidence at each stage.
Milestones, tasks, and remediation
Stage gates ensure learners progress only after meeting defined criteria: pre-clerkship, clerkship, and internship-like stages. For each stage, administer a test that combines a structured checklist, an OSCE-style station, and a real-world task under supervision. Require demonstration in areas such as gynecology and womens health, emergency resuscitation, and interprofessional teamwork. Target 85% pass on the checklist, with inter-rater reliability above 0.75. Collect evidence in a central form and allow learners to submit again after remediation. Remediation cycles occur within six weeks and results used to adjust training plans. Quarterly data reviews identify bottlenecks and adjust thresholds. Provide timely feedback and practical tips to supervisors and learners to accelerate improvement.
Facilities Upgrade: Lab Networking, Virtual Simulation, and Data Capture Systems
Upgrade the lab networking backbone to 10 Gbps links among core sites, then roll out virtual simulation and data capture in three phases. Phase 1 (june–august) connects the main laboratories, the mother education wing, and the aran research suites, deploying a 40 Gbps spine with redundant fiber paths and zero-touch provisioning. Phase 2 (september–december) expands to satellite labs across petrograd campus and adds edge compute for on-site instrument control. Phase 3 (january–june) implements full data governance workflows, unified access management, and external partner integrations. The programme allocates about $3.5 million for hardware, licenses, and staff training, with milestones linked to the opening events. The decision prioritizes genetic labs and clinical-practical spaces used by doctors across faculties; to participate across disciplines, teams will engage in nprove pilots.
Invest in a unified lab network fabric: 2 core switches at 10 Gbps, 4 edge switches, and 20 access switches, plus 2x 40 Gbps uplinks to the data center. Enable SDN-based orchestration and QoS for instrument control, streaming data, and parallel compute tasks; synchronize time with IEEE 1588 PTP to protect measurement integrity. Implement 2N redundancy for resilience and rapid failover. The nprove toolkit will automate provisioning, monitoring, and alerting, reducing manual toil by 40% in the first year. Budget lines include roughly $1.2 million for gear, $0.6 million for licenses, and $0.4 million for security, with a 24-month warranty and clear supplier milestones. This setup enables participation across labs and remote clinics, and it supports cross-campus data flows without latency spikes.
In the virtual simulation layer, deploy 3 high-fidelity suites with 12 stations each (36 seats total) and 2 GPU-based render clusters configured for real-time anatomy and procedure rehearsals. Allocate 120 TB NVMe storage for active models and 1 PB nearline for archives. License core simulators for 12 months with modular add-ons for genetics counseling (genetic) and rehabilitation scenarios, including rugby-related injury protocols. Integrate with the existing learning management system to track attendance, performance, and debrief notes, with results feedable into the mother education modules and clinical-practical training records for the faculty.
For data capture, link LIMS with EHR systems across hospitals using HL7/FHIR interfaces; structure metadata to capture instrument provenance, experiment conditions, and result lineage. Maintain исто/очник data streams with a clear data dictionary, audit trails, and role-based access controls. Implement automatic data tagging at capture points and enable cross-institution sharing under approved research programmes. Stores and backups follow a defined retention schedule (seven years for clinical data in line with regulations). The system supports data provenance requests (источник) and ensures that data can be traced from source to publication, with regular reviews by the data governance board. The team received favorable feedback from the associate dean and was awarded preliminary approvals for cross- campus data collaboration, reinforcing the overall scientific-practical aim of the programme and its data strategy.
Overall, the upgrades target a tight integration of network, simulation, and data layers to empower doctors across departments, expand research partnerships (including petrograd-linked centers), and accelerate publishing-ready results. Opening demonstrations will showcase real-time instrument control, AI-assisted debriefs, and end-to-end data capture workflows, inviting participation from the faculty, students, and external collaborators. The planned timeline aligns with the june milestones and is structured to accommodate quick iterations on requirements, enabling the possible scale-up as usage grows and more devices join the network.
Indoor Lambing System: Productivity Metrics, Welfare Checks, and Knowledge Dissemination

Install a sensor-based dashboard to track key farm results daily: births, losses, and ewe condition. Set clear alert thresholds so staff respond promptly, and use the data to adjust feeding and handling routines before issues escalate.
Metrics and Welfare Signals
In a unit with dense indoor pens, collect data on births per 100 ewes mated, live-born rate, pre-weaning mortality, and weaning weight. For a mid-size facility around 1,000 ewes, aim for near 170-190 live lambs per 100 ewes joined, pre-weaning losses below 8%, and weaning weights around 11-14 kg at 40-60 days. Track ewe body condition score (BCS) around 2.5-3.5 on a 1-5 scale; monitor udder health and teat integrity; assess lamb vigor at birth and colostrum uptake in the early hours after birth. Use sensor data on ambient conditions and pen density to identify stress periods; respond with adjustments in ventilation or pen grouping. When anomalies appear, trigger rapid vet checks; plan for rare medical procedures only if obstetric complications arise. The host animal health program should connect to clinical notes from the farm team and the local clinic, and the data should be accessible to staff across shifts to support timely decisions.
Knowledge Sharing and Training
Share results through simple reports and on-farm drills; develop short training modules for new staff and for routine refreshers; use an internal knowledge base to capture case studies on handling dystocia, colostrum management, and early weaning decisions. Build a learning loop with a clear delegation of responsibilities: who records data, who investigates alerts, and who coordinates with the veterinary team. Distribute materials to field teams, clinic partners, and research partners to encourage practice improvement and informed discussion on best methods for indoor lambing systems.

コメント